A roadmap into clinically relevant eHealth development

Are you aspiring to enter the eHealth sector? What opportunities are left in a market that already has over 165,000 Apps? Where to start? How to avoid creating another eHealth solution that sinks to the bottom of the barrel?
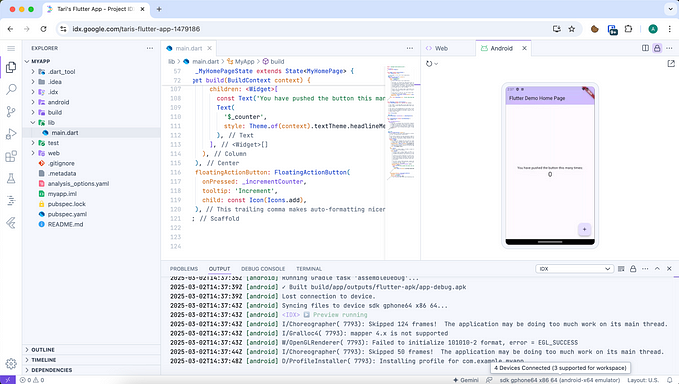
In a recent review of existing eHealth Apps, roughly two thirds of available offerings were identified as targeting personal wellbeing, with one third focused on disease management. This is illustrated in the graph below, taken from that source:

What’s striking about this summary is the mismatch between what we as customers (or patients) understand to be healthcare and the market offerings. Specifically, the market is satiated with fitness and wellbeing interventions rather than condition management solutions.
Currently, healthcare costs for managing long-term conditions account for 70% of total healthcare spending in the UK, with similar patterns across the developed world. Healthcare consumption is therefore dominated by individuals with long-term-conditions, at enormous cost — which means there is opportunity and need for innovation.
There are numerous routes into identifying opportunities and pitching meaningful digital solutions into healthcare. Here is a 7 step roadmap developed out of experience in this arena, to help get you started:
Step 1. Identify an existing problem

Spotting a great idea to work alongside existing healthcare is tricky, but essential. There are problems in the healthcare model, often recognised by those delivering it and/or those with unmet need or at risk. Reliably identifying these problems tends to rely upon a relationship with a service delivery body (organisation, team or clinician), an informed body (innovation funder, research team or academic literature) or patient representatives (charities, support groups etc).
Some ideas for creating these relationships:
- Attend conferences that are advertised to clinicians and the public, preferably where commissioners, purchasers and/or clinicians are presenting topics relating to eHealth. Take business cards and an open mind.
- Scan regional / national / international funding competitions for health innovation. Often these are promoted to businesses (SMEs primarily) or healthcare providers. If the latter, you may chase up local healthcare providers to enquire if they are interested and whether they have a technology partner.
- Attend local / national University conferences relating to eHealth, that are open to the public. Note down names of individuals that have completed exciting work that has not yet been digitised. Translating best practice into digital format is perhaps the easiest route into adoption.
- Monitor charity / support group social media around campaigns that may invite innovation. Make contact with them and/or clinical teams that could be linked via a technology partner. Don’t be afraid to act as the ring master — many clinicians are keen but embarrassed about not knowing how to start.
Getting a perspective on where clinical need exists is the priority.
Step 2. Capture the scale and characteristics of the problem.
Knowing the specific nature of a healthcare problem is critical. This may be regional, national or international. Some clinics are seeking a local solution for a local problem, whereas some funding competitions may be seeking an international scalable solution.
Where to source appropriate information:
- online: A lot of information relating to prevalence of diseases, costs and healthcare challenges is already published online.
- clinicians: Local clinical teams are usually the road into clinically relevant and specific data. They are often also linked to national representative bodies for their clinical specialities, which can provide more information and/or support.
- community sector: patient representative groups are usually plugged in to the successes and failures of current service delivery, against their own standards and national standards. They can often quickly summarise the needs of a service and summarise patient unmet need(s).
- service data: you could also ask local services if any AUDIT data exists, which summarises the performance of the service. Most services repeat these on regular intervals.
Try to summarise a statement about what the problem is, such as,
“60% of patients are not seen within the recommended time period in this setting with current medical resource. There is a national shortage of staff. The demand on services is expected to increase by 30% in the next 5 years.”
Obviously, there are many variations on this type of statement. But agreement between all parties, as to the ‘problem’ is the foundation of all future work.

Step 3. Map out existing patient journeys through healthcare (service design)
You need to consider existing healthcare as the familiar journey you are hoping to add to or replace. Understanding service delivery is imperative if you hope to see your innovation embedded. It’s not enough to have a great App, it needs to make sense to the public and any health provider it guides patients to or interacts with.
Themes to explore:
- What are the current patient stories, scenarios and journeys through healthcare, for this condition.
- Where are the gaps or failings, as perceived by the clinical teams AND by the patients, as these may differ).
- What is the ‘service’ paid to provide as an outcome (cure is rarely the outcome in long-term conditions — a form of support will be described).
- What expectations come with forms of ‘healthcare’ and with in supporting this particular health condition.
Through this process you may find pauses, dead-ends or loops in patient journeys that counter best practice for managing their health or frustrate any of the connected parties.
For example, many patients may be assessed every 6 months who don’t need to be — but the decision process is uninformed about which 20% are at risk and so all patients are seen. Patients may expect this level of service, find it pleasant and value the contact. However, the clinical need may not be there for 80% of patients and so costs and demand on services are high, unnecessarily.
It is areas like this that are ripe for innovation.
Step 4. Service innovation specification
At this stage, a specification of a required service need and possible solutions needs to be brainstormed with clinicians and patient representatives. Be open minded enough to recognise that the innovation may not be digital. There is no point pushing for an App, if a telephone call or a quick nurse appointment is more appropriate.
It is here where I see most innovation concepts lose momentum, as the idea was more related to the drive to justify an App rather than to evolve a service. The solution must invite an eHealth solution as it reduces time, offers better access to services, saves resource, monitors patients more often, triggers treatment, educates or some other metric that is recognised as invaluable in plugging the previously identified unmet clinical need.
Work with your stakeholders (patients, clinical team or charity) to find ways to not use technology. Repeated ask, do we really need eHealth to deliver this improvement? If you keep answering ‘yes’, then you have likely justified a hi-tech solution as opposed to the preferred low-tech alternative. The market will drift towards what is most sensible, cost effective and easiest to implement, making this step essential.
Step 5. Scope the market
Usually, this step is much earlier in a typical software innovation. I would argue that it is later in eHealth development. This is because eHealth must be tailored to the specific clinical need - and until you have identified this - you have no idea what you are scoping for.
For example, there are hundreds of epilepsy apps in the world, which may put off an uninformed developer who thinks the market is satiated, but no self-risk management tool existed (identified as a critical need) which led to us developing the award winning Epilepsy Self-Monitor solution.
Areas to scope:
- Scope competitors in the same arena. Do their interventions slot into your identified gap easily, and if so — are they already evidence based and at market. This may inform the scale of risk you are about to take but may also reveal where gaps have been left that leave clinical needs exposed.
- Technology trends — Consider all new technologies that you can feasibly leverage within your skillset. Does your proposed solution evolve with the addition of wearable tech or a new method of delivery?
- Success trends — What trends are appearing in respect to national procurement, innovation funding themes and publicised innovation implementation?
Step 6. Assess CRITICAL acceptability and added value perceptions.
Healthcare is famous for being slow to change. There is an entire industry of change-management professionals who coach change through the sector on regular occasions. Despite the constant change experienced by professionals, or because of it, clinical teams are very cautious of new promises and new ways of working.
Be sure to involve and collect impressions of your proposed innovation from the connected healthcare team / group. Explore how their jobs may change, what would be added, what would be taken away etc. Be sure that at the key levels, these changes are invited and recognised as good for the professionals and good for patients. Alienate the clinicians and you’ve lost your primary uptake strategies: referral to patients or embedding into services. It is better to sacrifice features if it results in a clinical appetite.
Step 7. Business Case
Last but not least (in fact, this should be in draft through most of the previous steps), you need a business case that maps the innovation design, impact on services, and cost implications against the original problem identified. This is your final pitch for procurement and a test of whether the idea has legs, in terms of becoming a component of clinical practice. All clinical service elements (equipment, staff, logistics) will have been procured via a business case. This is where you summarise all of the steps above into a coherent argument that proposes the likely positive impact.
Key phrases to keep in mind, include: feasibility, sustainability, maintenance, scalability, reliability, dissemination and security.
In conclusion…
eHealth is an opening market ripe for innovation. There remains an untapped potential to deliver key innovations into long-term condition management at varying geographical levels. This likely reflects an obscure route into this arena for non-clinical development teams, who seem to focus on more typical consumer health products. The 7 steps provided above is a brief introduction into becoming a provider of clinically embedded eHealth — most of it being extensions of normal ways of working for a diverse development team.
Next article (coming soon):
User stories and scenarios in eHealth — a 2 x 2 model.